World renowned ENT team at your service
+91 63668 88884 / 63668 88882

Case Studies
Avoid Canal Wall-Down Surgery – A Necessity To Prevent Cavity Problems And Preserve Hearing




An 11-year-old boy from Cuddapah (Kadapa, India) was presented to Bangalore ENT Institute with complaints of left ear discharge and reduced hearing in both ears for a one-year duration. The child also gave a history of bilateral ear pain on and off. The child had a past history of bilateral myringotomy and grommet insertion one year prior to the presentation of the current symptoms. The child did not give a history of nose or throat complaints.
On clinical examination, a retraction pocket was noted in the posterosuperior quadrants of both tympanic membranes. The fundus was not visualized. There was a thinned-out pars tensa in the anteroinferior quadrants of both tympanic membranes.
HRCT of the temporal bone showed a soft tissue density in the attic region with extension into the antrum and mastoid air cells. There was the erosion of the long process of the incus.
Audiometry and immittance showed mild conductive hearing loss on both sides with a ‘B’ type curve respectively.
HRCT of the temporal bone showed a soft tissue density in the attic region with extension into the antrum and mastoid air cells. There was the erosion of the long process of the incus. aditus. antrum and attic eroding the body and short process of incus and stapes suprastructure on the left side. The cholesteatoma sac with matrix was cleared completely during the procedure. Reconstruction of the ossicular system was done using reshaped incus and reconstruction of the tympanic membrane and attic was done using temporalis fascia and tragal cartilage.
Avoid canal wall-down surgery – a necessity to prevent cavity problems and preserve hearingollow-up. The child has shown signs of hearing improvement with a good graft uptake.
Stapedotomy – A One-Step Sure For Otosclerosis




A 30-year-old man presented to Bangalore ENT Institute with reduced hearing in both ears of 2 years duration which was gradually progressive. The patient did not give any history of ear pain, ear discharge, tinnitus or vertigo.
On clinical examination, both the tympanic membranes were normal. Pure Tone Audiometry showed a right severe mixed loss and left moderately severe mixed hearing loss. High Resolution CT scan of the temporal bone revealed a thickened footplate of the stapes. Patient was diagnosed to have bilateral otosclerosis.
Patient underwent Left Stapedotomy under general anaesthesia. Rosens incision was given. Tympanomeatal flap was elevated. Chorda tympani nerve was identified and retracted inferiorly. Posterosuperior meatal wall was curretted. Otosclerotic focus was identified in the fissula ante fenstrum. Stapedius tendon was cut. Incudostapedial joint was dislocated. Posterior crura was scored and separated from the footplate. Anterior crura was fractured. Fenestra of size 0.6 mm was created with a perforator. 4.25 mm piston was inserted and flaps were replaced.
Patients hearing improved post-operatively and is on close follow-up
Stage IV Cancer Larynx – Surgery Is Always The primary Treatment of Choice




A 75-year-old woman presented to Bangalore ENT Institute with a history of change of voice of one-year duration and sticky sensation in the left side of the throat along with shortness of breath and intermittent left ear pain of 3 months duration.
The change of voice was intermittent and temporarily used to resolve with antibiotics and steroids. However, the symptom was exacerbated with new onset of sticky sensation and shortness of breath which progressed over 3 months.
There was no history of odynophagia or aspiration. The patient complained of loss of appetite but no loss of weight. There was no history of fever with night sweats and hemoptysis. The patient was a known hypertensive on antihypertensive medications.
Examination of the neck revealed a firm, non-tender, mobile level IV neck node.
Laryngeal crepitus was present and laryngeal cartilage tenderness was present.
Examination of the larynx under anaesthesia revealed an infiltrative growth arising from the left ventricle with the following extensions
Superiorly - stopping short of the epiglottis
Inferiorly - stopping short of subglottis
Medially - involving the anterior 2/3 of the opposite false vocal cord
Laterally - involving the left aryepiglottic fold
Anteriorly - involving the left false cord and anterior commissure region
Posteriorly - Involving the left arytenoid
Interarytenoid and the post-cricoid area appeared free. The rest of the larynx and hypopharynx appeared free of growth. Glottic chink was inadequate. The left vocal cord and hemilarynx were fixed(on Hopkins telescopy before examination under anaesthesia). On palpation, the base of the tongue, tonsil and vallecula were not indurated.
Clinical diagnosis of malignancy of the hypopharynx T4aN1Mx Stage IVA
CECT of the neck revealed a 4.5 x 2.7 x cm mass lesion involving the left pyriform sinus, bilateral aryepiglottic folds, left lateral and posterior pharyngeal wall extending to the vocal cords and thyroid cartilage to the infraglottic region.
There was extra laryngeal extension across the thyroid cartilage involving the anterior and left anterolateral soft tissues in the infrahyoid region. There was an extension to involve the deep surface of the thyroid gland on the left.
The patient underwent a preliminary tracheostomy with examinati
on under anaesthesia and a biopsy revealed poorly differentiated squamous cell carcinoma.
Definitive surgery (Widefield laryngectomy) was performed under general anaesthesia Gluck Sorenson incision was given.
The subplatysmal flap was elevated. Lymph nodes(level IIA, IIB, III, IV) separated from the internal jugular vein along with the fascia. Right common carotid delineated and pedicles of superior and inferior thyroid artery identified and preserved after incising the strap muscles on the right side. Hypoglossal and spinal accessory nerves were identified and safeguarded. A medial gutter was created between the carotid and pharynx on the right side.
Thyroid and parathyroid were preserved on the right side. A similar procedure was carried out on the left side. However, the superior and inferior thyroid pedicle were ligated and left hemithyroidectomy and parathyroidectomy was done on the left side. In addition, level-V lymph nodes were dissected and removed on the left side.
The pharynx was entered after incising the suprahyoid musculature. The epiglottis was identified. Resection of the larynx along with partial pharyngectomy was done with a cancer-free margin. Constrictors are preserved on both sides along with mucosa of the left side. Neopharynx was created by an interrupted suture in 3 layers. Skin and subcutaneous tissue closure were done in 3 layers. The post-operative period was uneventful and the patient is on follow-up.
TYMPANOJUGULAR PARAGANGLIOMA – CAREFUL COMPLETE BLOODLESS DISSECTION OF THE TUMOR IS THE MANTRA; DURATION OF SURGERY IS IRRELEVANT!!




A 40-year-old woman from Mangalore was presented to Bangalore Skull Base Institute with reduced hearing in the left ear of 2 years duration with pulsatile tinnitus and giddiness of 1 year duration. Patient also had a history of voice change of 6 months duration. Patient did not give a history of ear discharge, bleeding from the ear or facial weakness. There was no evidence of difficulty in breathing, swallowing or regurgitation of food. There was no history of facial weakness.
Examination revealed a pulsatile, reddish mass in the left external auditory canal. Tympanic membrane was obscured by the pulsatile mass. Right ear was normal. Cranial nerve examination was normal.
Pre-operative audiometry revealed a moderate mixed hearing loss in the left ear with a “B” type curve on tympanometry. CECT of the temporal bone revealed an enhancing lesion arising from the left jugular foramen, protruding into left CP angle measuring 7.5 X 14 X 20mm with similar enhancement in the adjacent sigmoid sinus and internal jugular vein.
Bony erosions were noted involving the left jugular foramen. Bony erosion was noted in the proximal aspect of the left carotid canal and posterior wall of the left eustachian tube. Soft tissue densities were noted in the left eustachian tube and left middle ear suggesting a likely infiltration by the lesion.
CE-MRI revealed a T1W contrast-enhancing tumor originating from the left jugular foramen extending into the hypoglossal canal on the left side. Tumor extension was noted in the left internal jugular vein. Extradural extension into the left internal auditory meatus was noted. Tumor enhancement was also noted on T2W sequences.
Diagnosis of Left tympanojugular paraganglioma Fisch Classification De1 was made.
DSA and embolization revealed feeders from the left ascending pharyngeal artery and left occipital artery. Both vessels were embolized prior to surgery.
The patient underwent Infratemporal Fossa A approach for removal of left tympanojugular paraganglioma with OSIA implantation for rehabilitation of hearing. Intra-operatively the tumor was involving the middle ear(epi, meso, and hypotympanum extending into the Eustachian tube). Inferiorly the tumor was visualized involving the jugular foramen area and abutting the petrous carotid destroying the caroticojugular spine and medially extending extradurally into the IAM. The tumor was involving the jugular bulb with the involvement of the IJV lumen. Partial anterior transposition of the facial nerve resulted in a Grade III House Brackmann facial nerve palsy post-operatively.
The patient was discharged on postoperative day 5 and is currently on follow-up and recovering well.
POSTERIOR TYMPANOTOMY APPROACH FOR IATROGENIC MESOTYMPANIC CHOLESTEATOMA




A 35-year-old man from Bangalore presented to Bangalore ENT Institute with complaints of headache, giddiness, nausea and vomiting of 3 months duration and pain and tinnitus in the right ear of 2 months duration. He had a past history of surgery 4 times at various hospitals. On examination there was evidence of a post aural scar on the right side. However, the neotympanum was intact.
HRCT of the temporal bone revealed a lobulated soft tissue isointense mass located in the meso- and hypotympanum of the right ear. T1W MRI showed an isodense lesion in the right hypotympanum and DWI MRI revealed hyperdense mass localised in the right hypotympanum suggestive of cholesteatoma. There were features of a post-operative cavity with soft tissue in both CT and MRI.
Intra-operatively, we found a poorly defined cortical mastoidectomy cavity with fibrous tissue and overhanging cavity edges. The neotympanic graft from the previous surgery was intact with an ossicular strut on stapes footplate. The dilemma in proceeding with the surgery was based on the fact that the patient had a mild hearing loss from the previous surgery and any attempt to disturb the neotympanum or the ossicular strut could impact the hearing. Also, there was cholesteatoma in the meso- and hypotympanum which had to be addressed.
The patient underwent an intact canal wall revision cortical mastoidectomy and posterior tympanotomy approach for cholesteatoma clearance from the middle ear without disturbing the previous neotympanum or ossiculoplasty. Patient is on follow-up after surgery without any impact on hearing and symptomatically better.
Massive paraganglioma Stage Di2 – Staged surgery with hearing rehabilitation




A 49-year-old man presented to our clinic with blood-tinged right ear discharge, pulsatile tinnitus and progressive reduction in hearing of 2 years duration. On examination a pulsatile, polypoidal mass was completely occluding the right external auditory canal. The tympanic membrane on the right side was not visualized. Left ear was normal. Cranial nerves were intact. Pure tone audiometry revealed a profound hearing loss on the right side with normal left hearing.
CECT revealed a 3.6 x 3.39 cm contrast enhancing mass in the right jugular foramen region with extension into the horizontal petrous internal carotid artery with hemi-circumferenterial indentation of the ICA. MRI revealed a T1W contrast enhancing tumor with extension of approximately 1.2 cm in the intradural posterior cranial fossa. Embolisation of the feeding occipital artery, internal maxillary artery and ascending pharyngeal artery was done with internal carotid artery stenting.
CECT and MRI made a conclusive diagnosis of Right Tympano-jugular Paraganglioma Stage Di2. The patient underwent an Infratemporal fossa type A approach with blind sac closure following right internal carotid artery stenting and embolization of the tumor feeding vessels. Intra-operatively the tumor was infiltrating the facial nerve, internal jugular vein and indenting the lower cranial nerve complex. The facial nerve component was excised. External occlusion of the sigmoid sinus was performed along-with ligation of the internal jugular vein on the right side. The tumor was shaved off the lower cranial nerve complex and the horizontal petrous internal carotid artery. Near total removal of the tumor was performed. OSIA implant was placed in the occipital region. Staged removal for the intradural component and facial reanimation was advised for a later date. Histopathological examination confirmed the presence of paraganglioma. Patient has facial nerve paralysis HB Grade V and lower cranial nerve paresis immediately following surgery and is on regular follow-up
Never neglect a change in voice: It could be laryngeal cancer




A 69-year-old man presented to our outpatient clinic with a history of voice change and dysphagia of 20 days duration. He also had difficulty breathing for 5 days.
On clinical examination and direct laryngoscopy, there was an ulceroproliferative growth arising from right false cord extending medially to involve right aryepiglottic fold, medial and lateral wall of right pyriform fossa. Antero-superiorly, it involved the laryngeal surface of epiglottis on the right side and right pharyngoepiglottic fold. Posteriorly, it was involving the right arytenoid and inferiorly stopping short of the apex of the right pyriform fossa. The lesion was crossing the midline to involve the right true vocal cord. Right hemilarynx was fixed. There was widening of the laryngeal framework. No lymph nodes were clinically palpable. The final diagnosis was malignancy of the supraglottis T4aNoMx Stage Iva.
Contrast-enhanced CT scan confirmed the extent of the lesion. The patient underwent a preliminary tracheostomy followed by total laryngectomy, partial pharyngectomy, right hemithyroidectomy, bilateral selective neck dissection (level IIA, IIB, III, IV, VI) with primary reconstruction of the pharynx. Oral feeds were started on day 14 and the patient is doing well.
External Auditory Canal Cholesteatoma - Treated by Limited Mastoidectomy and Canal Wall Reconstruction




A 32-year-old woman presented to our clinic with chief complaints of blocked sensation and reduced hearing in the left ear of 3 years duration. On examination, the left external auditory canal was filled with keratin debris and the tympanic membrane was not visualized. She revealed a previous history of tympanoplasty for chronic otitis media- mucosal disease. HRCT of the temporal bone revealed a well defined lobulated mass lesion in the left external auditory canal. The lesion was causing a smooth scalloping of the external auditory canal and the mastoid and abutting the posterosuperior part of tympanic membrane. Pure tone audiometry showed a mild conductive hearing loss in the left ear.
The patient underwent left Conservative Mastoidectomy and Conchoplasty under General Anesthesia. Cholesteatoma matrix was removed in toto and a wide conchoplasty was done. Ossicles were normal. Temporalis fascia and cartilage were used to reduce the size of the cavity.
Patient is currently on follow-up 2 months post surgery and free of complaints.
Petrous Apicitis with Lateral Rectus Palsy




A 25-year-old gentleman presented with history of left sided severe headache of 1 month duration, diplopia in the left eye of 5 days duration following an episode of upper respiratory infection. He gave history of traumatic perforation of tympanic membrane with ear discharge one year prior to the current episode. He had history of reduced hearing following the trauma which gradually improved. He complained of occasional non pulsatile tinnitus and no history of vertigo.
Examination revealed delayed eye closure in the left eye, left lateral rectus palsy and left mild gaze induced nystagmus. Pupillary reflexes were normal. Corneal reflex was present. Tympanic membrane was normal. All lower cranial nerves were normal.
MRI and HRCT of the temporal bone revealed a soft tissue density in the left petrous apex region and epitympanum with erosion and otomastoiditis. Pure tone audiometry revealed a moderately severe mixed hearing loss in the left ear. He was diagnosed as a case of left petrous apicitis with lateral rectus palsy.
He underwent left subtotal petrosectomy with blind sac closure with OSIA implantation. Post-operatively, patients lateral rectus palsy resolved. Patient underwent switch-on for OSIA and currently is on regular follow-up and is free of symptoms.
A CLASSICAL CASE OF CARCINOMA TONGUE T2N0MX STAGE II TREATED BY WIDE EXCISION AND SELECTIVE NECK DISSECTION
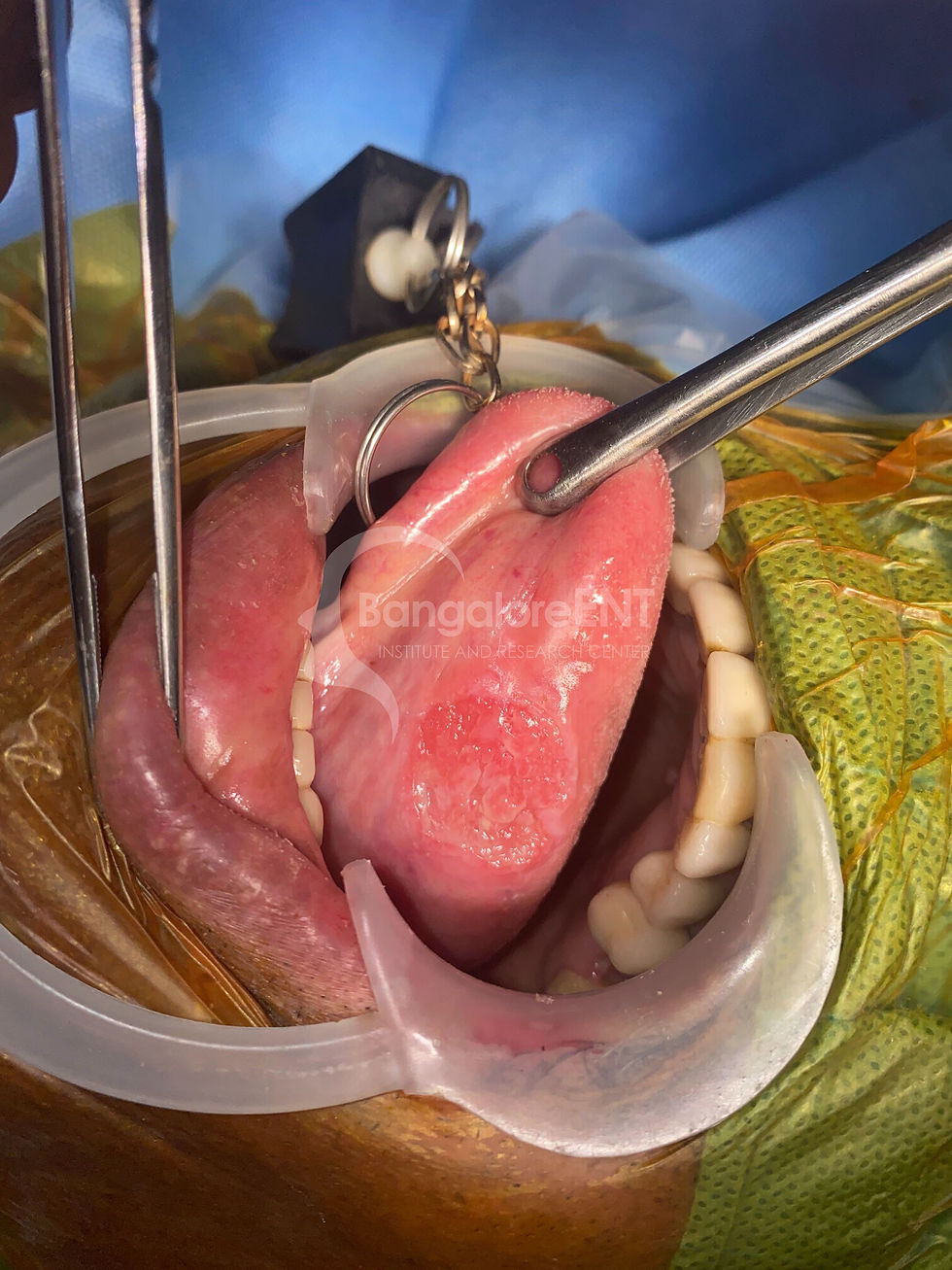


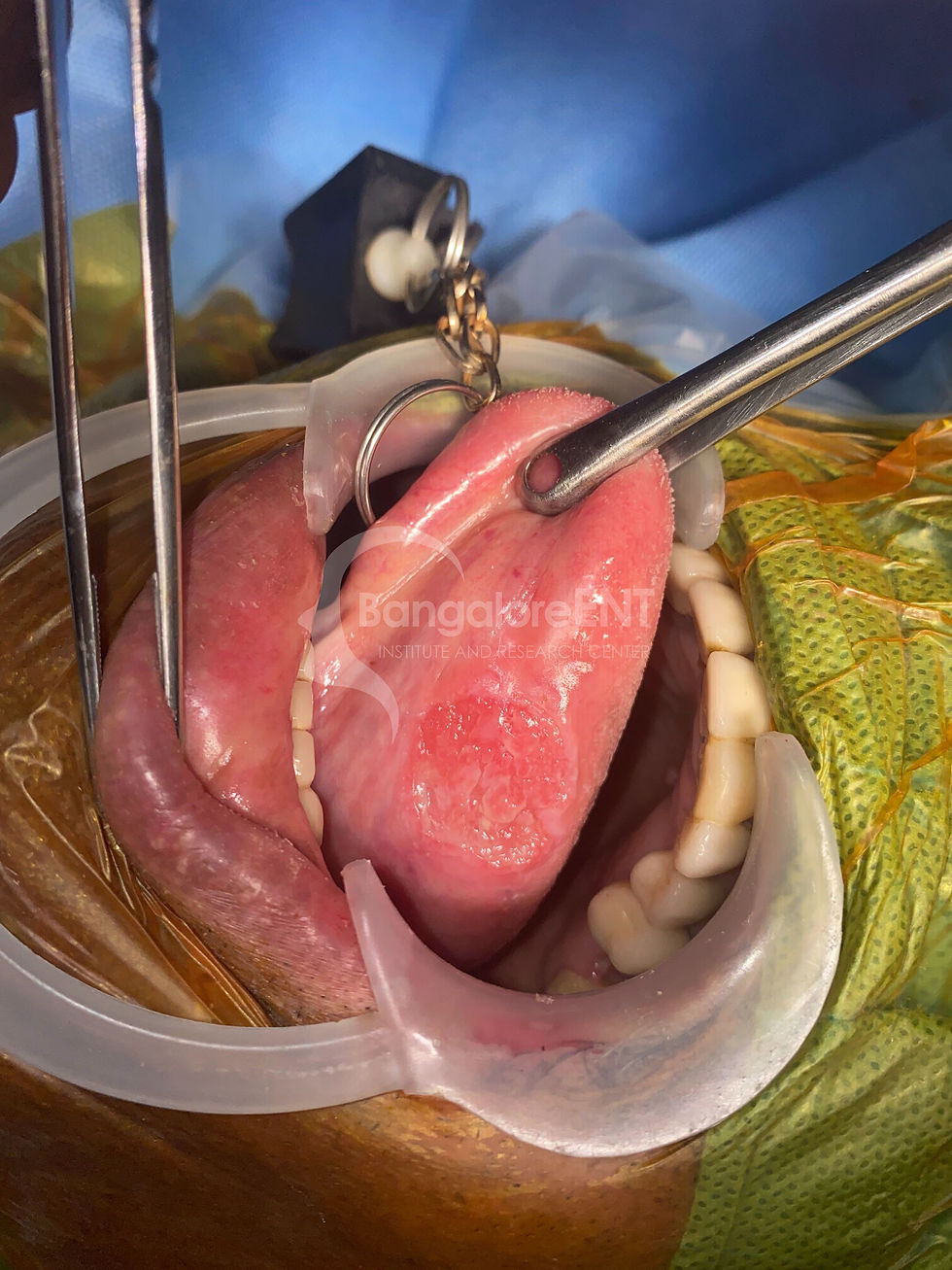
An 80-year-old gentleman presented with burning sensation and ulcer on the left side of the tongue of 4 months duration. He gave history of leukoplakic changes prior to the development of present lesion. Examination revealed a 3x2cms ulcerative lesion over the left lateral surface of the tongue, without overt underlying induration. Sub centimeter, soft lymph nodes were palpable in the left level IIA level.
CECT neck revealed a superficial lesion without significant deeper extension at the site of the ulcer. There was no definitive involvement of the extrinsic muscles of the tongue. A level II lymph node of size 9mmx7mm was observed. Biopsy from lesion revealed a histopathological diagnosis of moderately differentiated squamous cell carcinoma.
He underwent wide excision of the tumor with selective neck dissection on the left side (Level IA, IB, IIA, IIB and III). Neck dissection specimen showed multiple lymph nodes. HPE revealed that margins were free of tumor and lymph nodes were negative at all levels. Patient is currently on follow-up and free of symptoms.
A RARE CASE OF MULTIPLE HEAD AND NECK PARAGANGLIOMAS MANAGED WITH INTRALUMINAL ICA STENTING AND TUMOR RESECTION PRESERVING ALL THE LOWER CRANIAL NERVES




Head and paragangliomas are extremely rare tumors arising from the paraganglionic tissue of the nerves, with carotid body tumor being the most common in occurrence followed by tympanomastoid and tympanojugular paragangliomas and the least common of all being the vagal paraganglioma. Multicentricity is well documented and so is the multiple co-existing varieties. Here is a case of bilateral carotid body tumor with a vagal paraganglioma on one of the sides.
A 35-year-old woman from Bangladesh presented with a longstanding history of recurrent throat irritation, dry cough, foreign body sensation in the throat, for over 3 years, which subsided on taking antibiotics by her local physician. She underwent an ultrasound guided FNAC of the neck swellings, as suggested by her treating physician, which was suggestive of reactive lymph nodes. The patient, however, due to persistence of the symptoms, was advised an MRI neck with contrast, which revealed a enhancing neck mass bilaterally, suggestive of carotid body tumor. The patient was referred to Bangalore Skull Base Institute for further evaluation and management.
The subsequent MRI neck and skull base with contrast and TOF sequence, revealed a well-defined heterogeneously enhancing tumor extending from the carotid bifurcation up to the jugular measuring 6.2 x 4.2 x 2.7cms causing splaying of the ICA and the ECA, with >2700 encasement and luminal narrowing of the ICA in its superior cervical segment due to the compression by the lesion. A similar lesion measuring about 5.3 x 1.9 x 2.6cms arising from the carotid bifurcation extending superiorly up to the jugular foramen region on the left side. Preoperatively the patient had mild paresis of the right vocal unit showing compensated movements and mild hypoglossal deficit on the right side.
The patient was subjected to preoperative intraluminal overlapping C GUARD (INSPIRE MD) carotid stents of 6x40mm distally and 7x40mm proximally extending from origin of the right ICA (C1 segment) up to the origin of the petrous segment (C2 segment). The ECA feeders of the tumor were embolized by vascular coils. Tumor excision was planned through transcervical approach with mastoid extension getting the necessary infralabyrinthine exposure if required to access the jugular foramen area up to where the tumor is extended. Under the NIM eclipse (Medtronic) nerve monitoring system, the facial (CN VII), Glossopharyngeal (CN IX), Vagus (CN X), spinal accessory nerve (CN XI) and the Hypoglossal nerve (CN XII) were monitored all through the surgery.
Intraoperatively, there were two distinct tumors, one ovoid, ~3x4cms tumor at the carotid bifurcation, and a fusiform, 6x6.5cms tumor, of similar consistency (relatively posterior to the one at the carotid bifurcation) in proximity, abutting the Vagus nerve, but distinctly separable from the nerve, with prominent narrow caliber vasculature around the tumor nerve interface. The Vagus nerve showed strong neural activity at 0.5mA distal to the tumor limit and good neural activity at 2mA at its more proximal portions. The entire tumor was meticulously dissected and separated from the whole length of the Vagus nerve, and the tumor towards its superior most limit was closely abutting the upper cervical sympathetic trunk. The tumor however had no component extending into the jugular foramen region.
All cranial nerves were completely preserved anatomically and functionally, as confirmed by the nerve stimulator at the end of the procedure. The Vagus nerve showed good neural activity at 2mA when stimulated at its exit from the skull base, and the Hypoglossal nerve showed good neural activity at 2mA at the end of the procedure. The entire procedure was uneventful and so was the postoperative phase of the patient. The postoperative CT scan showed total tumor resection. The postoperative functional endoscopic evaluation of swallowing (FEES) showed minimal aspiration of liquids and solids well tolerated. The tumor on the left side is staged to be operated once the glottic compensation is completely achieved.
Intraluminal stenting of the carotid system and preoperative embolization, when done meticulously renders a clear advantage of total tumor resection and transposition of the vessels plausible, which also remarkably increases the probability of cranial nerve preservation, what should be of supreme importance especially in cases of bilateral craniocervical paragangliomas
INTACT CANAL WALL MASTOIDECTOMY IN A CASE OF TYMPANOMASTOID PARAGANGLIOMA(STAGE B3)




Tympanomastoid paragangliomas arise from the inferior tympanic or the mastoid canaliculi. It is a slow growing tumor with the property to invade neighbouring structures. Surgery is the treatment of choice in tympanomastoid paragangliomas.
A 38-year-old woman presented to the outpatient department with pulsatile tinnitus in the left ear of 3-years duration with intermittent blood-stained ear discharge. She also complained of gradually progressive reduced hearing in the left ear. Patient did not have history of vertigo, facial weakness, ear pain. There was no history of aspiration, dysphagia, hoarseness of voice, headache, alteration in taste. Family, personal and past history were insignificant.
On Examination, a red fleshy pulsatile mass was visualised in the left exernal auditory canal. Tuning fork tests revealed a moderate conductive hearing loss. Nose, Throat and Neck examination were normal. Cranial nerves were clinically intact. HRCT of the temporal bone (0.2 mm) revealed a soft tissue density in the left hypotympanum extending into the meso- and epitympanum into the aditus superiorly and eroding the horizontal carotid canal suggestive of Modified Fisch classification B3 Tympanomastoid Paraganglioma.MRI of the Temporal bone revealed low- to intermediate intensity on T1W and high intensity on T2W signals. The mass was seen abutting the left horizontal petrous carotid. Pure tone audiometry revealed a moderately severe conductive hearing loss on the left side.
Patient underwent an intact canal wall mastoidectomy with clearance of the tympanomastoid paraganglioma, canalplasty and cartilage tympanoplasty (Type II). The procedure was uneventful with an unremarkable perioperative period. The patient is currently on annual follow-up.
SUBTOTAL PETROSECTOMY WITH COCHLEAR IMPLANTATION IN A CASE OF TEMPORAL BONE SKULL BASE OSTEOMYELITIS




Skull base osteomyelitis is an aggressive condition with a high mortality rate, occurring in immunocompromised elderly individuals, especially with coexisting comorbidities like diabetes mellitus.
A 65-year-old male, a poorly controlled diabetic, with a longstanding history of fetid discharge from both his ears for close to two years, with a history of left sided facial palsy, which recovered with conservative management 1 year ago. He was being treated conservatively for bilateral CSOM by several physicians. The patient developed right sided facial palsy of HB grade IV about 4 months later. HRCT temporal bones of 0.2mm sections revealed bilateral temporal bone osteomyelitis. The disease on the right side extensively involved the retroparotid area and the jugular area in the infra-temporal fossa. The middle ear involved ossicular chain erosion, with intact stapes superstructure, partial involvement of the carotid canal, and sequestration of the stylomastoid foramen. The disease on the left side involved the external auditory canal, middle ear with ossicular destruction and the mastoid cavity.
The patient was operated by infratemporal fossa approach type B (ITFA-B) with blind sac closure on the right side, with extensive granulations on the left side in the middle ear cavity around the round window niche, the cochlear implant was deferred to be implanted on the contralateral side (left side after disease clearance at a later stage). The patient was taken up for a staged subtotal petrosectomy and disease clearance on the left side 4 months later and simultaneous cochlear implantation by (round window insertion) in the same ear followed by blind sac closure. Both the procedures were uneventful, with an unremarkable perioperative period. The patient is on a 3-month intravenous antibiotic regimen followed by a 3 month oral antibiotic regimen.
ENLARGED TRANSLABYRINTHINE APPROACH AND SIMULTANEOUS IPSILATERAL OSIA IMPLANTATION FOR A CASE OF GIANT VESTIBULAR SCHWANNOMA




Vestibular schwannoma despite being relatively rare are one of the most common posterior fossa and the most common tumor of cerebello-pontine angle. They are very slow growing tumors with an estimated general incidence of about 1 new case per 100000 population in a year. Two predominant histological patterns Antoni type A and B are identified in vestibular schwannomas.This is a case of a giant vestibular schwannoma of the right CP-angle who underwent an extended translabyrinthine surgery (ETLS) with simultaneous hearing rehabilitation with Osia implantation. A 41-year-old male patient presented with reduced hearing and tinnitus on his right side, which was gradually progressive over 7 months, with associated giddiness, especially while changingposition, and numbness over the right side of the face. A detailed clinical examination revealed absent right corneal reflex, with diminished sensation over the right V1, V2 and V3 dermatomes. The rest of otolaryngological examination and other cranial nerve examination was unremarkable. Radiologically the lesion was isointense to hypointense, hyperintense to isointense on T2, measuring 4.25x3.25x3.25, enhancement with contrast, with cystic changes in the center of the lesion, extending into the right internal auditory meatus, having significant compressive effect essentially over the middle cerebellar peduncle and entrapped CSF pockets on the prepontine and the cerebellopontine cisterns. The patient had moderate to severely compromised hearing in his right ear and normal hearing in his left ear preoperatively.
The patient underwent an extended translabyrinthine surgery with transapical extension type I (TA-I) with a simultaneous ipsilateral hearing rehabilitation with Osia implant under facial nerve
monitoring (NIM 2) and neuronavigation (Stealth system, Medtronic). The tumor resection was assisted with CUSA achieving more than 95% tumor clearance, with a thin sheaf of tumor abutting the facial nerve left behind and decompression of the entrapped CSF cisternal pockets. Hearing rehabilitation was done by Osia implantation. The entire procedure was uneventful, with an HB grade II at postoperative stay.
A Case of Bilateral Skull Base Osteomyelitis




A 59-year-old male, a known diabetic and hypertensive from Bengaluru presented with the imbalance and severe to profound hearing loss in both his ears since over a year and a half. He had a past history of longstanding persistent ear discharge in both his ears (right ear prior to left ear), for which has undergone a cortical mastoidectomy, a month after which he developed severe giddiness and was managed conservatively. After a period of subdued symptomatology, the ear discharge from both ears progressed once again leading to a cutaneous fistula behind his right ear. The patient was diagnosed having bilateral skull base osteomyelitis after having undergone a thorough systematic clinical and radiological evaluation at Bangalore Skull Base Institute (BSBI). The preoperative HRCT temporal bone revealed a postoperative right mastoid cavity, with haziness of the bilateral perilabyrinthine, retrofacial air cell tracts, and MRI suggestive of T2 hyperintensity of the left mastoid cavity, middle ear cavity, and the perilabyrinthine region with an evolving abscess of retropharyngeal prevertebral space. His preoperative VNG and cranial nerve examination were normal. The patient was planned for a subtotal petrosectomy for disease clearance and simultaneous ipsilateral cochlear implantation on the left side owing to more severe disease. Nevertheless, intraoperatively, owing to the extensive granulations in the perilabyrinthine region extending up to the internal auditory region, early erosions of the labyrinth and extension medial to the otic capsule, the procedure had to be improvised to transotic approach for accessing the more medial petrous compartment achieving total disease clearance. The procedure and the postoperative phase were unremarkable. A couple of months later the patient was taken up for disease clearance on the right side by a subtotal petrosectomy and cochlear implantation with a CI632 electrode. The intraoperative NRT was optimal, and the entire procedure was uneventful and so was his postoperative stay. The patient received intravenous antibiotics for three weeks and oral antibiotics for three months postoperatively.
An Interesting Case of Petrous Bone Cholesteatoma with Facial Palsy




Petrous bone cholesteatoma is a rare form of cholesteatoma involving more deeper confines of the temporal bone. The classic types include the supralabyrinthine, infralabyrinthine, infralabyrinthine apical, apical and massive labyrinthine. The preoperative status of the facial nerve plays a significant role in determining the surgical plan for disease clearance and managing the facial nerve outcome.
A 47-year-old male from Bangladesh, having an acute episode of right sided facial weakness a year back, which was diagnosed and managed as Bell’s palsy initially, and a plain MRI taken only a month later which revealed as a facial nerve schwannoma of the geniculate ganglion region. A repeat plain MRI scan taken again was diagnosed as a meningocele protruding into the right petrous bone.
The patient was referred to BSBI for further management, and a repeat contrast MRI and HRCT 0.2mm bone window suggested of a supralabyrinthine petrous bone cholesteatoma, erosion of the middle fossa dura, erosion of the superior aspect of the basal turn of the cochlea, erosion of the posterior fossa dura medial to the labyrinthine block, extension of the cholesteatoma into the internal auditory meatus compressing the facial nerve at its labyrinthine segment. The lesion was hypointense on T1 and hyperintense on T2 and showed restricted diffusion and no uptake of contrast. The patient was profoundly deaf on his right side, HB grade II facial weakness on the right side with no other cranial nerve palsy and intact tympanic membranes on both sides.
The patient was operated at by Dr Sampath Chandra Prasad Rao and Team at BSBI, Bangalore. The patient underwent a transotic approach with middle fossa transapical extension gaining a 3600 access of the internal auditory meatus. The labyrinthine segment of the facial nerve was cleared of the cholesteatoma and the facial nerve activity ensured with nerve monitoring at the end of the procedure. The cavity was obliterated with fat harvested from the abdomen and the wound closed in layers. The facial nerve function immediately after the recovery was HB grade II, and no CSF leak post-surgery. This case emphasizes on the role of specific radiological evaluation to arrive at the diagnosis.
Transotic Middle Fossa Approach with Simultaneous Ipsilateral Baha Implant and Masseter-facial Anastomosis for Extensive Petrous Bone Cholesteatoma




Petrous apex cholesteatomas are rather slow growing, very complicated and one of the extensive disease skull base surgeons commonly encounter. These deep seated cholesteatomas can occur either congenitally as a result of entrapment of the squamous epithelial cell rests within the deep confines of the petrous apex, or as an acquired pathology, where it is as a result of migration of the squamous epithelium from the external ear into the more medial domains of the temporal bone, or it could also be iatrogenic, as a result of seeding of the squamous epithelium into the middle ear during previous surgery, after which the disease grows into the petrous apex. The disease pattern can evolve within the petrous bone either as supralabyrinthine, infralabyrinthine, infralabyrinthine apical, apical, or massive labyrinthine cholesteatoma putting the neurovascular structures, the petrous ICA, the structures of the internal auditory meatus i.e., the labyrinthine segment of the facial nerve, the vestibulocochlear neural complex, seated in the lateral skull base of these areas in jeopardy.
Here is a case of 11-year-old female child, operated twice before for attico antral disease and a cochlear drill out and a blind sac closure the third time for disease clearance a couple of years back. Her recent MRI showing a lesion hypointense on T1 and Hyperintense on T2 in the petrous bone, in between the internal auditory meatus and the petrous ICA and middle fossa erosion. The disease clearance was achieved by transotic middle fossa approach with trans apical extension and complete disease clearance. The child was also implanted simultaneously on the same side with ‘cochlear BI300’ BAHA implant, and a simultaneous lateral canthopexy, tarsorrhaphy and masseter and facial end to side anastomosis.
Transotic Middle Fossa Approach with Simultaneous Ipsilateral Baha Implant and Masseter-facial Anastomosis for Extensive Petrous Bone Cholesteatoma




Petrous apex cholesteatomas are rather slow growing, very complicated and one of the extensive disease skull base surgeons commonly encounter. These deep seated cholesteatomas can occur either congenitally as a result of entrapment of the squamous epithelial cell rests within the deep confines of the petrous apex, or as an acquired pathology, where it is as a result of migration of the squamous epithelium from the external ear into the more medial domains of the temporal bone, or it could also be iatrogenic, as a result of seeding of the squamous epithelium into the middle ear during previous surgery, after which the disease grows into the petrous apex. The disease pattern can evolve within the petrous bone either as supralabyrinthine, infralabyrinthine, infralabyrinthine apical, apical, or massive labyrinthine cholesteatoma putting the neurovascular structures, the petrous ICA, the structures of the internal auditory meatus i.e., the labyrinthine segment of the facial nerve, the vestibulocochlear neural complex, seated in the lateral skull base of these areas in jeopardy.
Here is a case of 11-year-old female child, operated twice before for attico antral disease and a cochlear drill out and a blind sac closure the third time for disease clearance a couple of years back. Her recent MRI showing a lesion hypointense on T1 and Hyperintense on T2 in the petrous bone, in between the internal auditory meatus and the petrous ICA and middle fossa erosion. The disease clearance was achieved by transotic middle fossa approach with trans apical extension and complete disease clearance. The child was also implanted simultaneously on the same side with ‘cochlear BI300’ BAHA implant, and a simultaneous lateral canthopexy, tarsorrhaphy and masseter and facial end to side anastomosis.
VAGAL PARAGANGLIOMA -TRANSMASTOID INFRALABYRINTHINE CERVICAL APPROACH




The paragangliomas are rare tumors arising from the paraganglionic tissue. Making up for only 3% of all the paragangliomas and comprising ~0.6% of the head and neck tumors and only 0.03% of all the tumors is what makes these tumors more intriguing regarding their pattern and behavior. Carotid body tumors make up nearly 60% of the head and neck paragangliomas, the tympanojugular paragangliomas 40% and vagal paragangliomas <5%.
This is a case of a massive vagal paraganglioma in a 58-year-old male patient, presenting as a neck mass sans associated clinical symptoms. There was no cranial nerve deficit. Video laryngoscopy showed bilateral symmetrically completely mobile vocal folds. Functional endoscopic evaluation of swallowing (FEES) showed no deficits. The preoperative radiological imaging, MRA with time-of-flight sequencing (TOF) and contrast enhanced study, was consistent with highly vascular tumor with significant flow voids within, involving the right upper lateral cervical, parapharyngeal space, the right infratemporal fossa, abutting the petrous bone, right jugulo-carotid complex, displacing the right C1 (cervical) segment of the ICA anteriorly drawing active feeders from the ipsilateral subclavian artery and from the suboccipital artery.
The surgery was performed by Team Dr Sampath Chandra Prasad Rao, Bangalore Skull Base Institute, Bangalore. The tumor was preoperatively embolized, albeit partially (~30%) and was taken up for a transmastoid infralabyrinthine transcervical approach. A near total resection was achieved with a small tumor remnant on the C1 ICA left behind due to extensive vascular feeders to the tumor. (>98%, as assessed by post-operative CT volumetrics). The transmastoid infralabyrinthine transcervical approach gives a comprehensive control over the neurovascular structures, particularly the petrous ICA to deal with potential mishaps. The patient had a quick and an optimal recovery post-surgery.
AN INTERESTING CASE OF COCHLEAR IMPLANT AND MAGNET CHANGE




Despite the more recent and advanced cochlear implants being quite compatible with MRI, it is not unusual to come across complications during scanning such as partial or complete depolarization of the magnet, displacement of the implant electrode and pain, where the scan needs to be abandoned. Nevertheless, the disrupted implant needs to be addressed to put the implant back to its function.
Here we have an experience to share, where a child, having previously undergone cochlear implantation for her right ear, at a private center, was planned for left ear cochlear implantation at our center. Owing to the dilemma of the patient not being offered a simultaneous bilateral cochlear implantation during the first time, and lack of any previous medical reports, radiological images, the patient again had to be worked up. During the 1.5 tesla MRI scan, the child complained of severe, lancinating pain over her right temporal region during the scan. Following this, the processor was found to be dysfunctional and wouldn’t sustain in place, suggesting either magnet displacement or depolarization which rendered the child bilaterally deaf. One of the options was to install a reverse polarized magnet in the processor. Since the arrival of the magnet would have taken more than a couple of weeks, the child was planned for cochlear implantation on the left side without delay, along with exploration of the receiver stimulator bed of the existing implant on the right side.
The receiver stimulator bed on the right was approached a little posteriorly lest not to end up damaging the receiver while dissecting the soft tissue. The button magnet of the stimulator was found flipped over its belly, which was retrieved from its pocket. The magnet was also weak, suggesting depolarization, hence a new magnet was replaced in its place, and wound closed in layers. The cochlear implantation was completed uneventfully on the opposite side as planned.
Bilateral Cochlear Implantation (S.No 46)




Proven and agreed upon are the advantages of an early bilateral cochlear implant over being done on only one side, specifically for the better speech and language learning capabilities and unarguably better binaural sound perception, not to mention the enhanced brain and intellectual development of a born deaf individual. With an incidence of nearly 5700 cases for every million newborn children, congenital deafness bears a significant impact on our developing society, be it both economically and emotionally.
We this week have a case of a year and a half old, born deaf female orphan, who underwent a successful simultaneous bilateral cochlear implantation.
The psychomotor evaluation of the child preoperatively was satisfactory for her age. The radiological- HRCT temporal bones showed favorable anatomy and MRI was suggestive of bilateral normal morphology.
The procedure was posterior tympanotomy facial recess approach with extended cochleostomy on both the sides, the implants used were 'Nucleus profile plus with slim modular electrode CI632', the insertion of the electrode arrays complete and smooth. The procedures on both sides were uneventful. The post operative HRCT temporal bones done on POD-I confirmed the position of the implants.
Castleman’s Disease of the neck - No. 44




An 11-year-old girl presented with a gradually progressive isolated left side painless neck mass for 4 years. The physical examination showed 4x5 cm non tender, mobile, firm, well defined swelling in the neck at the level IV region extending up to the left supraclavicular region. Ultrasound sonography showed a 4x2x4 cms well-defined hypoechoic oblong mass with central and peripheral vascularization at the level IV region with multiple lymph nodes at level V. Computed tomography (CT) with contrast showed 4.8x4.6 cm well defined enhancing mass in left level IV region displacing the IJV anteriorly and CCA medially. Multiple enhancing enlarged lymph nodes seen in the left supraclavicular area. Two USG guided fine needle aspirations attempts were non-contributive. A surgical excision biopsy under general anesthesia was planned. The mass was abutting IJV anteriorly, CCA posteromedially, superiorly extending at the level of cricoid cartilage, posterolaterally up to posterior border of SCM. Few significant firm lymph nodes were also noted in level V. The extirpation was challenging as level IV and level V selective neck dissection was performed through a small curvilinear incision. Complete disease clearance was achieved with a good cosmetic outcome. The diagnosis of Castleman's disease was made based on final histological findings following which the IHC panel was sent. Patient is on regular follow up with no signs of recurrence.
GExtensive skull base osteomyelitis with prevertebral abscess managed by Infratemporal type B approach with subtotal petrosectomy and deep lobe parotidectomy.




A 74-year-old female from Bangladesh presented to us with complaints of excruciating left ear pain, tinnitus, and decreased hearing on the left side for 5months. The patient eventually developed ear discharge, facial asymmetry, and hoarseness of voice after 3 months. The patient was a known case of uncontrolled diabetes, hypertension, bronchial asthma, and chronic kidney disease.
The patient visited our center in Bangalore and was further evaluated. Audiological evaluation revealed severe SNHL on the left side and Mild SNHL on the right side. MRI scans revealed findings consistent with left otomastoiditis and temporal bone osteomyelitis with soft tissue inflammation in the infratemporal fossa and a small abscess in the left prevertebral longus capitus muscle of 1.1x0.9cm. CT scan revealed opacification of the middle ear, antrum, attic, and mastoid air cells with opacification and extensive soft tissue density with areas of bony erosions. Erosions are seen extending to the lateral margin of clivus and occipital bone adjacent to occipitomastoid suture and along anterior margins of the carotid canal and of sigmoid plate. The facial canal showed few areas of dehiscence in the region of middle ear.
Patient underwent Infratemporal type B approach with subtotal petrosectomy and deep lobe parotidectomy. Multiple microabscesses involving middle cranial fossa dural plate, presigmoid area, infratemporal fossa, retro facial area, jugular bulb area, tympanic segment of facial nerve, petrous carotid area, prevertebral area with frank pus and foramen spinosum. Extensive erosions seen over vertical petrous internal carotid artery and caroticojugular spine. Extensive disease clearance was achieved from hypoglossal canal area, infratemporal fossa and infralabyrinthine area.
Postoperative CT scan revealed complete disease clearance and patient had an immediate improvement of facial palsy. The patient is under follow-up and shows drastic improvement in clinical condition.
Giant Cell Tumor of the temporal bone excised via Infratemporal fossa approach type C (No. 41)




A 35-year-old male from Bangalore presented with left sided progressive hearing loss and ear pain for 3 months. He also had a history of trismus for 2 months. On examination, a reddish mass was seen filling the entire EAC. PTA revealed profound hearing loss of 90dB in the left ear and normal hearing in the left ear. HRCT and CEMRI temporal bone showed an ill-defined large expansile heterogeneous multiloculated cystic lesion measuring 6.6x5.1x5.5 cms in the left temporal bone. The lesion appears hypo intense on T1, hyperintense on T2 and FLAIR sequences. Patient underwent Infratemporal fossa approach type C. Frozen section showed Giant Cell Tumor. Total disease clearance was achieved, preserving the facial nerve in the Fallopian canal from the labyrinthine segment to stylomastoid foramen. Petrous ICA was decompressed along its entire length from its entry into the petrous bone to the foramen lacerum. Postoperative period was uneventful. Post op facial nerve function was normal. Patient is on regular follow up and on repeat scan there is no residual/recurrent disease.
Congenital Petrous bone cholesteatoma: Transotic petrosectomy with facial nerve decompression with right lateral canthoplasty.




A 35-year-old male presented with right sided long standing facial paralysis and progressive hearing loss for 10 years. Patient was diagnosed with Petrous bone cholesteatoma 2 years back and had undergone surgery via Middle Cranial Fossa approach elsewhere for the same. However, his facial nerve paralysis gradually worsened since then. On follow-up MRI with contrast, there was residual cholesteatoma in the petrous apex, IAC, encasing VII & VIII, and cochlea. The patient came to our center for further management. Otoendoscopy revealed an intact TM. Patient had HB Grade V facial nerve paralysis. Nerve conduction study showed severe right facial axonopathy. PTA revealed profound hearing loss 90dB in the right ear and normal hearing in the left ear. HRCT temporal bone showed a huge area of enhancing soft tissue density measuring 22x 10mm. CEMRI revealed diffusion restriction and T2 hyperintense signals in the right petrous apex causing bony erosions. The VIIth nerve in tympanic and mastoid segments was intact. Features were suggestive of residual petrous bone cholesteatoma on the right side . Patient underwent Transotic petrosectomy with facial nerve decompression with right lateral canthoplasty. Total disease clearance was achieved preserving the facial nerve in the fallopian canal from the labyrinthine segment to stylomastoid foramen, preserving the petrous internal carotid artery. Postoperative period was uneventful. Patient is on regular follow up with HB grade V facial paralysis and his facial nerve function is expected to recover further due to the facial nerve decompression.
A tale of epistaxis : case of capillary hemangioma of temporal bone




A 48-year-old male patient from Bangladesh presented with epistaxis. Multiple investigations including endoscopy and radiological evaluation confirmed the primary source of bleed as a mass lesion involving the left temporal bone and eustachian tube. His Pure Tone Audiometry revealed hearing sensitivity within normal limits in the right ear and moderate mixed hearing loss in the left ear.
The patient underwent Subtotal Petrosectomy with blind sac closure with ipsilateral BI 300 4mm implant with abutment. Post-operative recovery was uneventful. Histopathology revealed the lesion to be a capillary hemangioma. Four weeks after the surgery the patient was fitted with Baha 5 Power processor.
Case of Stage IV A (T4aN3M0) squamous cell carcinoma of oral cavity resected enbloc by commando operation and reconstructed with PMMC flap




73 years old male patient from Bangalore presented with a swelling over the right side of neck with proliferative lesion arising from the floor of the mouth, noticed 20 days back. The lesion and neck nodes were painless, hard in consistency, and did not bleed on touch. The patient gave a history of tobacco chewing and smoking for over 40 years.
On examination of the oral cavity, the proliferative lesion was noted involving the right ventral surface of the tongue, floor of the mouth, tonsil, mandible and an impeding ulcer of the skin over the submandibular area. Neck examination revealed multiple enlarged neck nodes in levels I, II, and III, which are hard in consistency, and the size of the largest neck node was 3x 4cm in level II with fixation of overlying skin. Biopsy confirmed the diagnosis of a well differentiated squamous cell carcinoma of the oral cavity.
Radiological evaluation revealed an irregular, infiltrative, and slightly lobulated margin, heterogeneously enhancing 3.4x 3.1x 4.2 cm mass lesion located in the right submandibular gland in the submandibular space. The lesion was seen extending to involve the posterior part of sublingual space and right hyoglossus muscle, right tonsillar fossa upto platysma.
MRI also showed bilateral multiple enlarged heterogeneously enhancing abnormal lymph nodes at level IB, II and III, the largest measuring up to 1.9 x 1.3 cm at the right and 2.4 x 1.7 cm left at level II.
The patient underwent en bloc resection of the oropharyngeal lesion by commando operation and radical neck dissection with tongue flap and PMMC flap reconstruction.
Postoperative histopathology confirmed the diagnosis of well differentiated squamous cell carcinoma and all margins were negative and free of malignancy. Patient is free of the disease after 1 year.
Nasopharyngeal carcinoma cT3N0Mx: Right endoscopic medial maxillectomy and nasopharyngectomy




A 64 year old male from Assam, presented with symptoms of right sided nasal obstruction with epistaxis on and off since 8 months. Diagnostic nasal endoscopy revealed non pulsatile mass medial and posterior to middle turbinate filling the entire right nasal cavity and right choana extending partially to left choana. Mass was friable and bled on touch. Pure tone audiometry revealed normal hearing on both sides with A type Impedance audiometry. Both contrast-enhanced paranasal sinus CT scan and MRI showed heterogeneously enhancing 3.2x3x5cm lesion arising from right posterolateral wall, filling the right choana and part of left choana. There is extension to the region of Fossa of Rosenmuller with minimal involvement of prevertebral muscles. Bilateral FESS with Right endoscopic medial maxillectomy and nasopharyngectomy was performed. Postoperative period was uneventful. Histopathology was consistent with undifferentiated nasopharyngeal carcinoma. Patient underwent post-operative radiotherapy. Immediate post op scan has been shown.
Giant Ossifying fibroma of temporal bone: Infratemporal Fossa Approach Type B with Sub temporal craniotomy




A 35 year old male from Jharkhand, presented with symptoms of right ear block, decreased hearing and tinnitus for six months. Otoendoscopy revealed non pulsatile mass filling entire middle ear and bulging into EAC. VII, IX, X, XI, XII cranial nerve examination was normal. Pure tone audiometry revealed 90dB profound hearing loss on right side. MRI contrast revealed lobulated T2 hyperintense lytic lesion arising from right petrous apex and temporal bone. CT with contrast revealed hypodense non enhancing lesion of the petrous bone. Right Infratemporal Fossa Approach Type B with Sub temporal craniotomy was done. Postoperative period was uneventful without any cranial nerve paralysis/paresis. Histopathology was consistent with Ossifying Fibroma. Post-op follow scan 6 months later showed no residual or recurrence of disease.




A 14-month-old baby boy from Bangalore was diagnosed with congenital bilateral sensorineural hearing loss. BERA revealed bilateral severe-to-profound hearing loss. Baby was fitted with hearing aids on both the sides and was given auditory verbal therapy for a period of 3 months. There were no benefits seen using the same. Hence, he was recommended to undergo bilateral cochlear implant surgery. CT & MRI revealed no anatomical abnormality on both the sides. Bilateral Cochlear Implantation was performed with Cochlear Nucleus CI632 Implant. Intra-operative monitoring revealed Impedance and Neural response telemetry within normal limits (NRT).




A 51-year-old male patient presented with a one-year long history of nausea, vomiting and imbalance. The episode got precipitated following a minor RTA, and was associated with gradual loss of hearing with poor speech discrimination and tinnitus in the left side. MRI revealed a heterogeneously enhancing solid tumor of 3.69cmX2.99cmX3.52cm size with cystic areas in the left CPA. The tumor was seen widening the fundus of left IAM, which is a feature highly suggestive of vestibular schwannoma. A Translabyrinthine approach for excision of giant Vestibular Schwannoma was performed with simultaneous ipsilateral OSIA Implantation for hearing restoration. Post-surgery patient recovered well with a HB grade II facial paralysis. Upon switch on of the OSIA implant, the patient was able to hear normally with good speech discrimination, in both quiet and noisy environment.




Tympanojugular paraganglioma Type C3: Infratemporal fossa type A approach
A 69-year-old female, presented with profuse left side ear bleed since five days. Patient had profound hearing loss and pulsatile tinnitus for which she had undergone canal wall down mastoidectomy elsewhere for apparent removal of Tympanojugular paraganglioma in 2015. Patient also had compensated left vocal cord paralysis. Otoendoscopy revealed reddish bulged TM with reddish mass protruding from the inferior quadrant. Pure tone audiometry showed 90dB profound hearing loss on the left side. MRI with contrast showed heterogeneously enhancing lesion (salt and pepper appearance) centered in the left jugular foramen with erosion of the caroticojugular spine, partially encasing the petrous ICA. CT scan showed lytic destructive expansile lesion centered in the left jugular foramen causing erosions, eroding the petrous carotid, hypotympanum and petro-mastoid temporal bone. Embolization of the feeding vessels was done 24 hours before surgery. An Infratemporal fossa type A approach was performed, where the tumour was removed completely along with anterior transposition of the facial nerve. Post op event was uneventful. Patient developed HB grade III facial nerve paralysis and is expected to recover further.
Giant Multinodular Goiter


A 59-year-old female from Yemen presented with a huge swelling on her neck which was progressively increasing in size over the past few years. She had associated difficulty in swallowing solids and a constant feeling of a lump in her throat. She did not complain of any breathing difficulties or change in voice. The preoperative evaluation confirmed the diagnosis of multinodular goiter which on ultrasound scan was approximately 10x 12cm with euthyroid status.

A 59-year-old female from Yemen presented with a huge swelling on her neck which was progressively increasing in size over the past few years. She had associated difficulty in swallowing solids and a constant feeling of a lump in her throat. She did not complain of any breathing difficulties or change in voice. The preoperative evaluation confirmed the diagnosis of multinodular goiter which on ultrasound scan was approximately 10x 12cm with euthyroid status.

A 59-year-old female from Yemen presented with a huge swelling on her neck which was progressively increasing in size over the past few years. She had associated difficulty in swallowing solids and a constant feeling of a lump in her throat. She did not complain of any breathing difficulties or change in voice.
The preoperative evaluation confirmed the diagnosis of multinodular goiter which on ultrasound scan was approximately 10x 12cm with euthyroid status.
The patient underwent total thyroidectomy under general anesthesia. Intraoperative images are shown below. Specimen revealed a huge multinodular goiter on the left side which was 14x 20cm in size with multiple small nodules in the right gland. Bilateral parathyroid gland and laryngeal nerves preservation was achieved.
The postoperative period was uneventful with preservation of normal voice and calcium levels. The patient was discharged on thyroid hormone supplements.
Skull Base Osteomyelitis




Skull base osteomyelitis due to impacted foreign body in the petrous bone: Subtotal petrosectomy with facial nerve decompression with simultaneous ipsilateral cochlear implantation for hearing restoration
A 56 year old lady presented with right ear pain, ear discharge, bleeding and facial deviation for 1 month. Patient had a past history of severe hearing loss for several years and was offered hearing aid. During the trial, ear mould was inserted deep inside the EAC following which she developed symptoms. A week later she developed facial paralysis, following which a local ENT surgeon removed ear mould debris from the EAC and referred the patient to our center. Otoendoscopy revealed large central perforation with mucopurulent discharge and granulations in the EAC. Patient had HB Grade V facial nerve paralysis. Pure tone audiometry revealed profound hearing loss 90dB in the right ear and 75dB severe SNHL in the left ear. HRCT temporal bone revealed soft tissue density in the middle ear and EAC with demineralization of the tympanic segment of the facial nerve with ? foreign body along the horizontal petrous carotid and eustachian tube. Patient underwent Subtotal petrosectomy with facial nerve decompression with simultaneous ipsilateral cochlear implantation for hearing restoration. The foreign body which was an ear mould material was removed completely. Post surgery, recovery was uneventful. She was put on long term antibiotics as per our SBO antibiotic protocol. The CI switch on was done after 3 weeks, following which the patient’s hearing has been restored successfully. Over 3 months, her facial nerve function has marginally improved and it is expected to improve further.
Parotid Tumor Abutting Facial Nerve




A 23-year-old female presented with left parotid swelling. She had incidentally noticed the swelling 1 year back which was increasing in size progressively over the past few months. FNAC of the lesion proved phleomorphic adenoma. On examination, the lesion was obvious and measured 3cm x 2cm over the angle of the mandible left side with normal facial nerve.
Further radiological evaluation revealed a lesion abutting and displacing the facial nerve.
The surgery went as planned and under high resolution with facial nerve monitoring, the tumor was dissected out from the facial nerve. Subcuticular sutures were placed and wound closure done after hemostasis.
Postoperatively the facial nerve was normal as confirmed intraoperatively when 0.5mAmp was giving a good response. Her sweet smile was intact after surgery, as was promised to her!
Translabyrinthine approach for Giant Vestibular schwannoma with simultaneous Ipsilateral OSIA implantation for hearing restoration


A 51-year-old male patient from Dubai presented with a one-year long history of nausea, vomiting and imbalance. The episode got precipitated following a minor RTA, and was associated with gradual loss of hearing with poor speech discrimination and tinnitus in the left side. MRI revealed a heterogeneously enhancing solid tumor of 3.69cmX2.99cmX3.52cm size with cystic areas in the left CPA. The tumor was seen widening the fundus of left IAM, which is a feature highly suggestive of vestibular...

A 51-year-old male patient from Dubai presented with a one-year long history of nausea, vomiting and imbalance. The episode got precipitated following a minor RTA, and was associated with gradual loss of hearing with poor speech discrimination and tinnitus in the left side. MRI revealed a heterogeneously enhancing solid tumor of 3.69cmX2.99cmX3.52cm size with cystic areas in the left CPA. The tumor was seen widening the fundus of left IAM, which is a feature highly suggestive of vestibular....

A 51-year-old male patient from Dubai presented with a one-year long history of nausea, vomiting and imbalance. The episode got precipitated following a minor RTA, and was associated with gradual loss of hearing with poor speech discrimination and tinnitus in the left side. MRI revealed a heterogeneously enhancing solid tumor of 3.69cmX2.99cmX3.52cm size with cystic areas in the left CPA. The tumor was seen widening the fundus of left IAM, which is a feature highly suggestive of vestibular schwannoma. A Translabyrinthine approach for excision of giant Vestibular Schwannoma was performed with simultaneous ipsilateral OSIA Implantation for hearing restoration. Post-surgery patient recovered well with a HB grade II facial paralysis. Upon switch on of the OSIA implant, the patient was able to hear normally with good speech discrimination, in both quiet and noisy environment.
CPA Epidermoid


22 years old male patient presented with intermittent episodes of giddiness and tinnitus left ear with left ear block since six months. Otoendoscopy revealed intact TM. VII, IX, X, XI, XII cranial nerve examination was normal. Pure tone audiometry revealed bilateral hearing sensitivity within normal limits. MRI Brain and temporal bone with contrast showed well defined non-enhancing T1 hypointense and T2 predominant hyperintense diffusion restricting lesion in the left CPA suggestive...

22 years old male patient presented with intermittent episodes of giddiness and tinnitus left ear with left ear block since six months. Otoendoscopy revealed intact TM. VII, IX, X, XI, XII cranial nerve examination was normal. Pure tone audiometry revealed bilateral hearing sensitivity within normal limits. MRI Brain and temporal bone with contrast showed well defined non-enhancing T1 hypointense and T2 predominant hyperintense diffusion restricting lesion in the left CPA suggestive....

A 22 years old male patient presented with intermittent episodes of giddiness, tinnitus and blockage in the left ear for six months. Otoendoscopy revealed intact TM. VII, IX, X, XI, XII cranial nerve examination was normal. Pure tone audiometry revealed bilateral hearing sensitivity within normal limits. MRI Brain and temporal bone with contrast showed well defined non-enhancing T1 hypointense and T2 predominant hyperintense diffusion restricting lesion in the left CPA, suggestive of an epidermoid (22x27x22mm). Translabyrinthine approach for the excision of the CPA epidermoid with blind sac closure and BI300 4mm implant was placed on the mastoid occipital region. Postoperatively, the patient had HB grade II facial nerve paralysis with no intracranial complications. Histopathology was consistent with epidermoid.
Temporal Bone Squamous Cell Carcinoma




A 74 year male, known diabetic, presented with blood tinged left ear discharge and ear pain since one month. Patient had a long standing history of bilateral ear discharge, decreased hearing left ear more than the right and occasional giddiness on and off since 20 years. There was no history of facial nerve paralysis. He was on oral antibiotics, analgesics on and off for the same. Otoendoscopy revealed left EAC aural polyp obscuring the view of Tympanic membrane, right ear showed subtotal perforation with edematous middle ear mucosa. There were no palpable neck nodes. Cranial nerve examination including Facial Nerve was found to be normal. Biopsy of the aural polyp revealed moderately differentiated squamous cell carcinoma. PTA showed profound hearing loss in the left ear (>90 dB) and severe sloping mixed hearing loss in the right ear (85dB). Subtotal temporal bone resection with selective (level V, IIA, IIB) neck dissection and partial parotidectomy with blind sac closure was performed. BI300 4mm implant with cover screw placed on the mastoid occipital bone. Post op Facial nerve status was HB Grade II. Patient is planned for radiotherapy.
Massive Petrous Bone Cholesteatoma




A 45 year old female from Bangladesh with complaints of decreased hearing in the left ear for three months with previous surgery probably cortical mastoidectomy for CSOM elsewhere. Otoendoscopy showed sagging of posterior and superior wall of EAC. VII, IX, X, XI, XII CN were normal. PTA showed moderately severe mixed hearing loss in left ear with distorted smooth pursuit with overshooting saccades. Cranial nerve examination found to be normal. CT & MRI with contrast was done. Diagnosis: Massive Petrous Bone Cholesteatoma with Meningoencephalic herniation
Patient underwent Subtotal Petrosectomy with blind sac closure with meningoencephalic herniation repair under general anesthesia. Post op period uneventful. Post op Facial nerve normal.